SGLT2 Inhibitors (Sodium-Glucose Co-transporters 2 Inhibitors) are increasingly being used in the treatment of patients with Diabetes Mellitus Type 2. SGLT2 Inhibitors are preferred when the diabetic patient has any of the following signs and symptoms:
- Hypertension
- edema or fluid overload
- Obesity or overweight
- Cardiac disease and heart failure
- Diabetic nephropathy
- Hyperuricemia
The sodium-glucose-glucose cotransporter 2 inhibitors (SGLT2) reduce blood glucose by increasing urinary glucose excretion.
Unlike most other antidiabetic medicines, SGLT2I do not have any effect on insulin secretion and hence they seldom cause hypoglycemia.
Furthermore, they induce some degree of weight loss because of the Glucose (calories) lost through the urine.
| You may also like to read: |
Mechanism of action of SGLT2 Inhibitors:
The SGLT2 receptors are expressed in the proximal tubules of the kidneys. These receptors mediate the reabsorption of approximately 90 percent of the filtered sugar load.
SGLT2 inhibitors increase renal glucose excretion and thereby lower the elevated levels of glucose in patients with type 2 diabetes.
This therapy causes osmotic diuresis as a result of filtered glucose that is not allowed by the drug to enter back into the systemic circulation.
Moreover, even though the SGLT2 inhibitors currently in development almost completely block proximal tube glucose reabsorption (A1C), the measured inhibition is less than 50 percent based on urine glucose excretion.
SGLT2 inhibitors lower plasma glucose levels by blocking reabsorption. This decreases as plasma glucose levels fall.
In the absence of hypoglycemia-causing therapies, they don’t usually cause hypoglycemia. SGLT2 inhibitors moderately lower blood pressure and weight.
| You may also like to read: |
SGLT2 Inhibitors Indications (Uses):
The treatment of Diabetes mellitus type 2 should begin with a balanced and healthy diabetic diet, weight loss, aerobic exercise, and other lifestyle changes, importantly reducing stress.
The usual first line of therapy is metformin in most patients. However, some patients might not tolerate metformin or have contraindications to its use.
Furthermore, the degree of hyperglycemia is another deciding factor when choosing anti-diabetic medicines. Important side effects or complications that might occur as a result of using SGLT2 inhibitors might also limit their use.
The following group of patients may benefit the most from using SGLT2 Inhibitors:
- In patients suffering from an overt atherosclerotic cardio disease (CVD), not reaching glycemic targets with metformin or lifestyle modifications:
Recommendation: Use empagliflozin, Dapagliflozin, and canagliflozin but not Ertugliflozin.
- In patients suffering from heart failure who are not able to reach glycemic goals using metformin and lifestyle modification:
Recommendation: Use Empagliflozin, Dapagliflozin and Canagliflozin
- In patients with a urine albumin-to-creatinine ratio greater than 300 mg/g and an estimated glomerular filter rate [eGFR] of 90mL/min/1.73m2:
Recommendation: Use Canagliflozin or Dapagliflozin, or Empagliflozin.
Other General Recommendations Include:
- As a third-line treatment …
- in patients with inadequate glucose control on two oral medications (eg, Metformin or sulfonylurea), if a combination of metformin/insulin is not an option.
- As a third-line treatment …
- in patients who are not well controlled by metformin or insulin therapy. Patients in whom glucagon-like peptide-1 receptor agonists (GLP-1) are contraindicated and increasing insulin doses would cause weight gain
- As an adjunct …
- in patients who have not been able to control their metformin and are unable or unwilling to consider injectable therapy.
| You may also like to read: |
Contraindications and precautions when using SGLT2 Inhibitors:
Patients with hyperglycemia should not take SGLT2 inhibitors in the following situations.
- Type 1 diabetes mellitus
- Type 2 diabetes with estimated glomerular filter rate (eGFR) of:
- Less than 60mL/min/1.73 m² (ertugliflozin),
- Less than 45mL/min/1.73 m² (dapagliflozin or empagliflozin), and
- Less than 30mL/min/1.73 m² [canagliflozin]
- Prior diabetic ketoacidosis (DKA).
Furthermore, patients with more severe renal disease may experience a lower SGLT2 benefit. SGLT2 inhibitions do not have the same glycemic benefits as patients with less severe kidney disease.
SGLT2 inhibits are not recommended to be initiated in patients with eGFR thresholds. All SGLT2 inhibitors should be stopped if eGFR is 30 mL/min/1.73 m².
SGLT2 inhibitors are effective in treating kidney disease. However, they have been shown to be beneficial for patients with eGFR greater than 30 mL/min/1.73 m².
| You may also like to read: |
When should SGLT2 Inhibitors be avoided?
Patients with these conditions should not be given SGLT2 inhibitors. This is because they are more likely to become seriously ill.
- Frequent bacterial infections of the urinary tract or genitourinary yeast infections.
- Low bone mineral content and high risk of falling and fracture.
- Foot injury (eg, neuropathy or foot deformity), and/or history of foot ulceration.
- Factors that predispose to DKA include type 2 diabetes (ketosis-prone), pancreatic insufficiency, and drug or alcohol addiction.
The SGLT2 inhibitors may cause mild dehydration. They should not be used in combination with any other medications that could predispose you to acute kidney injury.
Drugs that should be avoided or used with caution with SGLT2 Inhibitors include:
- NSAIDs, nonsteroidal anti-inflammatory drugs,
- Diuretics,
- Nephrotoxic drugs like aminoglycosides and heavy metals
- Corticosteroids
In addition, certain diseases that could predispose you to acute renal damage should be promptly treated including hypovolemia, heart failure, and liver disease.
| You may also like to read: |
Which SGLT2 Inhibitor should you choose?
Empagliflozin Vs Dapagliflozin Vs Canagliflozin Vs Ertugliflozin?
Before initiating treatment with an SGLT2 Inhibitor, it is important to consider the co-morbid conditions first. The major comorbid conditions that might influence the use of one SGLT2 Inhibitor over the other are:
- Atherosclerotic Cardiovascular diseases
- Heart failure
- Kidney disease
Atherosclerotic Cardiovascular diseases:
In diabetic patients with atherosclerotic cardiovascular diseases, empagliflozin and Canagliflozin are preferred.
Empagliflozin in a dose of 10 mg and 25 mg was studied in a randomized clinical trial that comprised a total of 7020 patients.
The primary composite outcome was death from a cardiac cause, nonfatal myocardial infarction, and nonfatal stroke. The primary outcome occurred in 10.5% of the studied patients in the empagliflozin group compared to 12.1% in the placebo group (P:0.04) [Ref].
The rates of myocardial infarction and strokes were similar in both groups. However, the rates of hospitalization for heart failure, death from any cause, and death from cardiovascular causes. This is shown in the chart below:

The cardiovascular outcomes in Canagliflozin-treated patients were similar, however, patients in the canagliflozin-treated patients were at an increased risk of developing fractures and a greater number of patients had lower limb amputations.
This effect was not seen in patients treated with empagliflozin.
| You may also like to read: |
Heart failure in Diabetic patients:
All SGLT2 inhibitors have been proven to have a beneficial effect in type 2 diabetic patients who have comorbid heart failure or kidney disease.
Most cardiologists prefer Dapagliflozin (Forxiga) because of its non-selective nature. Dapagliflozin is 5000 times less selective than Empagliflozin for SGLT2 receptors. It also inhibits SGLT1 receptors which are predominantly present in the GI tract and the heart.
In a study conducted on patients with NYHA Class II, III, or IV heart failure and an ejection fraction of 40% or less, Dapagliflozin in a dose of 10 mg significantly reduced hospitalizations for heart failure and cardiovascular death rates.

| You may also like to read: |
Diabetic Patients with Kidney disease:
In diabetic patients with kidney disease (Diabetic Nephropathy), all SGLT2 Inhibitors have been shown to reduce the progression of kidney disease.
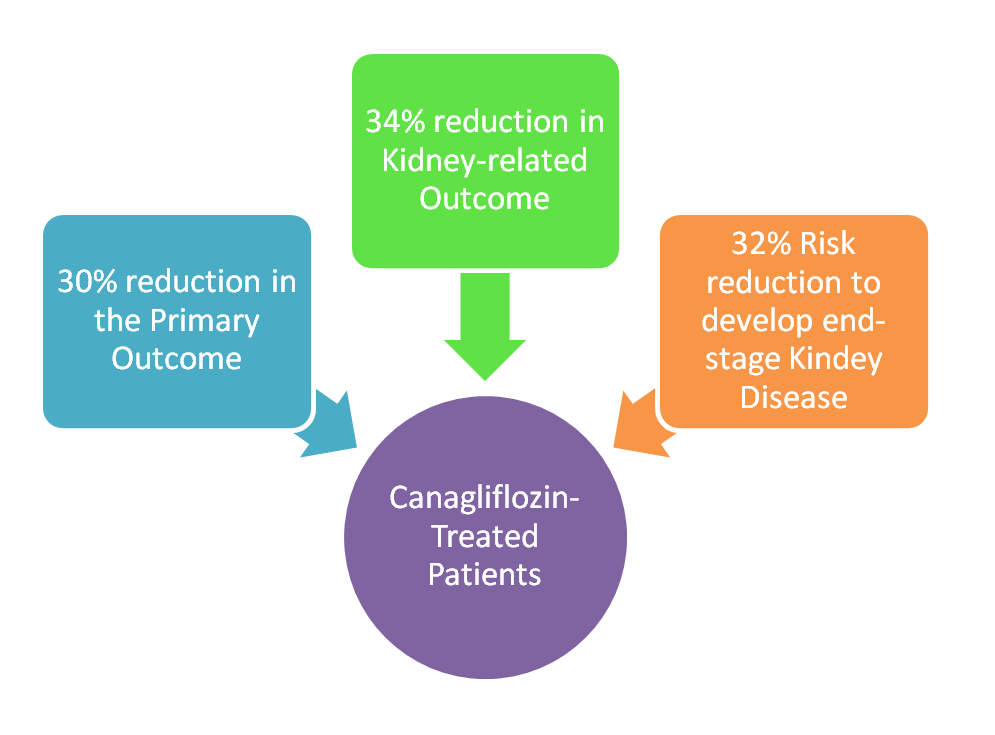
Canagliflozin in Kidney Disease:
Treatment with Canagliflozin in a dose of 100 mg was compared with a placebo in patients with albuminuric kidney disease and a GFR of 30 to 90 ml/minute in one study [Ref]. The primary outcome was defined as:
- a composite of end-stage kidney disease including patients requiring dialysis or kidney transplantation, or a sustained eGFR of less than 15 ml per minute per 1.73 m2,
- an increase in the serum creatinine to double that of the baseline, or
- death from renal or cardiovascular causes
The results of the study were as follows:
- There was a 30% reduction in the relative risk of the primary outcome in patients who received Canagliflozin.
- There was a 34% relative risk reduction in kidney-related outcomes that included patients who died from kidney disease or had a doubling of the serum creatinine from the baseline.
- The relative risk of developing end-stage kidney disease was lowered by 32%.
| You may also like to read: |
Dapagliflozin in patients with chronic kidney disease:
Dapagliflozin was also studied in patients with Chronic Kidney disease with or without Diabetes. The primary outcome was a decline in the GFR of 50% or more, patients developing end-stage kidney disease, or death from kidney-related or cardiovascular causes.
The primary outcome was observed in 9.2% of the patients who were treated with Dapagliflozin vs 14.5% in the placebo-treated patients.
More deaths occurred in the placebo-treated patients (6.8%) vs patients treated with dapagliflozin (4.7%) [Ref].
| You may also like to read: |
Empagliflozin in Kidney Disease:
Empagliflozin recently got fast-track FDA approval in patients with chronic kidney disease.
It was observed to reduce the risk of composite renal outcomes (dialysis, renal transplantation, or a profound, sustained reduction in the eGFR) in 1.6% of patients compared to 3.1% in the placebo group (hazard ratio, 0.50; 95% CI, 0.32 to 0.77).
There was also a reduction in the continued decline of eGFR in the empagliflozin group compared with placebo (–0.55 ml per minute per 1.73 m2 per year vs –2.28 ml per minute per 1.73 m2 per year) [Ref].
| You may also like to read: |
Glycemic efficacy of Canagliflozin vs Empagliflozin Vs Dapagliflozin Vs Ertugliflozin:
SGLT2 Inhibitors have not been directly compared in clinical trials. HbA1C reduction with SGLT2 Inhibitors is usually between 0.3 to 0.6%.
Empagliflozin reduced HbA1C by 0.54% and 0.60% when administered in a dose of 10 mg and 25 mg respectively [Ref].
Dapagliflozin reduced HbA1C by 0.21% +/- 1.14 compared with placebo 0.04 +/- 1.29 [Ref].
Among the SGLT2 inhibitors, Canagliflozin 300 mg is considered superior to other SGLT2 Inhibitors. The glycemic efficacy of SGLT2 Inhibitors is ranked as:
Canagliflozin 300 mg > Empagliflozin 25 mg > Dapagliflozin 10 mg
Evaluation of the patient before initiating SGLT2 Inhibitors:
Before starting an SGLT2 inhibition, it is important to assess the patient’s volume and renal function (serum creatinine with eGFR). Hypovolemia must be corrected prior to treatment initiation with an SGLT2 Inhibitor.
Liver function should be monitored especially when initiating treatment with canagliflozin and dapagliflozin.
All patients, particularly those who are being given Canagliflzoin and patients who are at risk of falls and fractures should have a Dexa scan done and bone density measured.
Patients who use insulin or insulin secretagogues (sulfonylureas and glinides), may need to reduce their insulin doses in order to lower the risk of hypoglycemia.
| You may also like to read: |
SGLT2 Inhibitors Dosing:
Before treatment initiation, monitor renal functions. In advanced kidney disease, SGLT2 inhibitors are less effective. Patients with reduced eGFR should not be initiated on SGLT2 inhibitors if the eGFR is in the following ranges:
- eGFR 30 mL/min/1.73 m2 or less:
- Do not initiate SGLT2 Inhibitors.
- eGFR of 30 – 45 ml/min/1.73m²:
- Canagliflozin may be given, Other SGLT2 inhibitors should be avoided.
- eGFR of 45 – 60 ml/min/1.73m²:
- Treatment with all SGLT2 inhibitors can be safely initiated except for Ertugliflozin.
- eGFR of more than 60 ml/min/1.73m²:
- Can safely initiate treatment with SGLT2 Inhibitors.
After the initial therapy, the decision about increasing the dose should be made based on tolerance and adverse effects.
| You may also like to read: |
Canagliflozin Dose:
Canagliflozin can be taken orally before eating. To achieve your glycemic goals, the initial dose should be 100 mg. It can then be increased to 300 mg daily.
Patients with moderate renal impairment (eGFR 45-59 mL/min/1.73 2) should not take more than 100 mg daily.
In patients with liver disease, dose adjustment is not required in mild to moderate hepatic impairment, however, patients with severe hepatic impairment should not receive canagliflozin.
Dapagliflozin Dose:
Dapagliflozin (10mg once daily) is safe to take with or without food. Patients with active bladder cancer are not advised to take it.
Patients with severely reduced liver function should start at 5 mg per day.
Empagliflozin Dose:
Empagliflozin can be taken orally one time daily, with or without food. To achieve your glycemic goals, the initial dose of empagliflozin is 10 mg per day.
It can be increased to 25mg daily. Patients who experience a persistent fall of eGFR (45 mL/min/1.73 m²) should stop taking empagliflozin. Patients with hepatic impairment may be able to take empagliflozin.
Ertugliflozin Dose:
Ertugliflozin can be taken with or without food once daily, in the morning. To achieve your glycemic goals, the initial dose of 5 mg is taken once daily.
The maximum daily dose can be increased to 15 mg. Patients who experience a persistent fall of eGFR (60 mL/min/1.73 m²) should stop taking ertugliflozin.
| You may also like to read: |
Monitoring Required When using SGLT2 Inhibitors:
During SGLT2, it is important to monitor more than just glycemic indices like A1C and fasting sugar. Also, renal functions, blood pressure, and volume status should be closely monitored.
Renal function Monitoring:
- eGFR >60mL/min/1.73m²:
- Monitor serum creatinine after every three months. If stable, it can be checked annually or as indicated by a physician.
- eGFR between 45-60 mL/min/1.73 m2:
- Check serum creatinine every three to six months, or as indicated by the doctor.
Glycemic indices Monitoring:
SGLT2 inhibitors may increase hypoglycemia risk in patients who take insulin or insulin secretagogues.
Patients taking insulin or insulin secretagogues should monitor their fasting glucose and pre-meal fingerstick glucose during the first few weeks after initiation or dose escalation.
If blood glucose levels are below 80 mg/dL, insulin dosing should be reduced by 10-20% and insulin secretagogue doses by 50 percent.
Measure HbA1C every three months until the glycemic goal is achieved. Patients who meet glycemic goals are measured at least twice annually.
However, it is best to continue measuring HbA1C quarterly for patients who have changed their therapy or are not meeting those goals.
Monitoring for Adverse events:
Patients on SGLT2 inhibitors need to be closely monitored for symptoms such as genitourinary and foot infections.
Patients should have a lipid profile measured at baseline and three to six monthly, especially in patients with co-morbid cardiovascular and renal diseases.
A statin may be indicated in patients with abnormal lipid profiles to reduce the risk of developing atherosclerotic cardiovascular diseases.
| You may also like to read: |
In Conclusion:
SGLT2 Inhibitors (Empagliflozin, Dapagliflozin, Canagliflozin, and Ertugliflozin) are used for controlling hyperglycemia in diabetic individuals.
These drugs are preferred in patients with kidney and heart diseases. However, treatment should be individualized and adverse drug reactions should be considered when initiating treatment with an SGLT2 Inhibitor.




