Diabetic heart failure is one of the common causes of heart failure resulting in hospitalization and death nowadays.
Because symptoms of chest pain and shortness of breath may not be present on initial presentation, they may be overlooked and misdiagnosed.
The lack of symptoms and misdiagnosis might make it fatal. Even if the patient survives, he/ she can have long-lasting symptoms that restrict his/ her mobility and productivity.
How Prevalent is Diabetic Heart Failure:
In the United States, more than 29 million adults have type 2 diabetes while 6.5 million have heart failure and these numbers are expected to rise over time.
These conditions often occur together which severely affects patient outcomes, quality of life, and expenses due to their adverse outcomes.
Patients having diabetes mellitus are more prone to develop heart failure even when other risk factors like hypertension, age, and hypercholesterolemia are adjusted, as compared to those without diabetes.
The Framingham Heart Study suggests that diabetes mellitus independently increases the risk of Heart Failure up to 2-fold in men and 5-fold in women compared with age-matched controls [Ref].
A recent study suggested that 44% of patients hospitalized for HF have diabetes mellitus and it is an independent risk factor for the development of heart failure [Ref].
Advanced age, hypertension, hyperlipidemia, coronary artery disease, family history, lifestyle, and insulin use all are independent risk factors for developing heart failure in diabetic patients.
If we consider individual diseases, heart failure is more lethal and has a poor prognosis so the priority of treatment lies in the management of heart failure in diabetic patients.
| Read: |
Risk Factors for Diabetic Heart Failure:
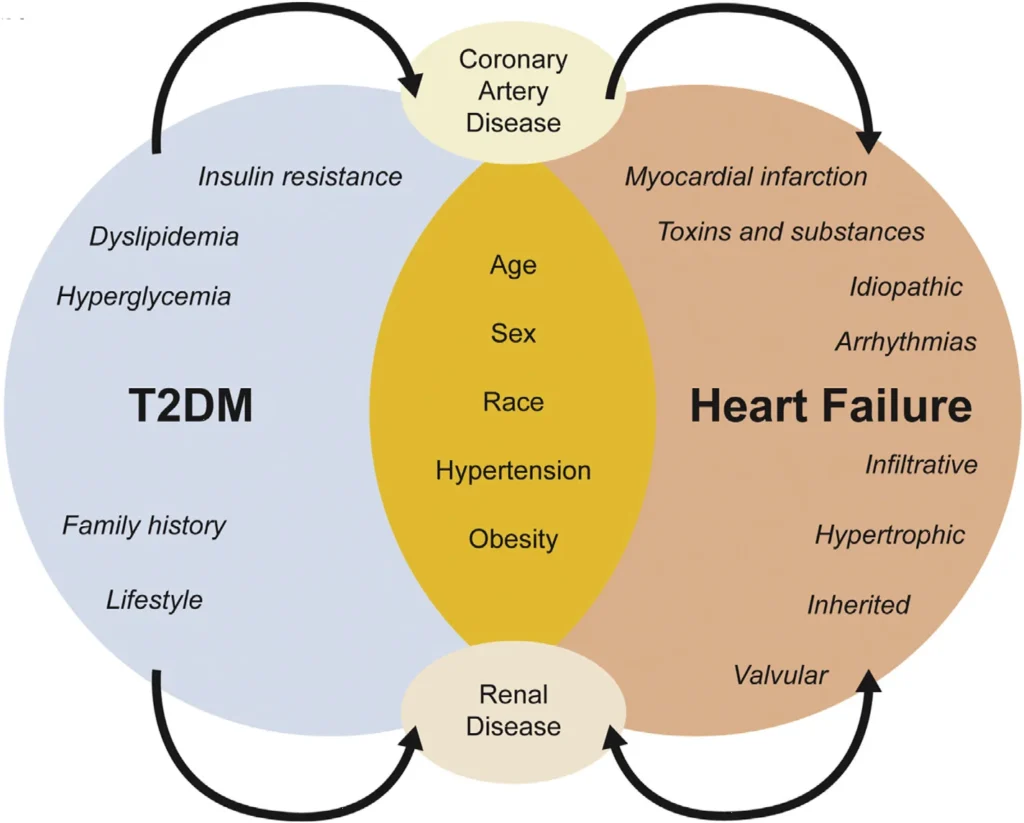
Diabetics have an increased risk of developing heart failure not only because of coronary artery disease but because of improper glucose metabolism which causes structural and functional abnormalities in cardiac function.
The impaired cardiac glucose metabolism and the switch of glucose to FFA oxidation that occurs in the diabetic heart have a significant negative effect on cardiac contractility and functioning.
Thereby inducing left ventricular systolic and diastolic dysfunction even in the absence of coronary artery disease (CAD) or structured heart disease.
The mechanism involved is decreased glucose transport and oxidation, increase in the use of free fatty acid, decreased sarcolemmal calcium transport, and alterations in myofibrillar regulatory contractile proteins which leads to a decrease in energy reserves and efficiency of heart function.
Hyperglycemia and insulin resistance impair cardiac function by cross-links in collagen molecules due to glycation end products leading to increased fibrosis and myocardial stiffness.
Diabetes mellitus significantly increases the risk of recurrent hospitalizations for heart failure and the duration of hospital stay in patients with heart failure, and it is associated with significantly higher mortality compared with those without diabetes.
Diastolic heart failure or HFpEF (heart failure with a preserved ejection fraction) is a common cause of heart failure in diabetic patients. It occurs as a result of myocardial stiffness and impaired filling.
Most recently approved antidiabetic drugs such as Empagliflozin, Dapagliflozin, and Semaglutide have been found to treat these patients. They have now been approved in patients with HFpEF even in the absence of diabetes.
| Read: |
Symptoms of Diabetic Heart Failure:
The symptoms of diabetic heart failure are not very different from the symptoms of heart failure in non-diabetic individuals.
However, diabetics may have more severe symptoms than non-diabetics. Here are the symptoms of diabetic heart failure:
- Shortness of breath (dyspnea) when you exert yourself or when you lie down (orthopnea) you may wake up at night due to dyspnea
- Fatigue and weakness
- Swelling (edema) in your legs, ankles, and feet due to the collection of fluid in the body
- Palpitations (rapid heartbeat)
- Persistent cough or wheezing with white or pink blood-tinged phlegm
- Very rapid weight gain from fluid retention
- Lack of appetite and nausea
- Dizziness
- Confusion
- Chest pain if your heart failure is caused by a heart attack
Symptoms of right-sided heart failure are different than left-sided heart failure. Here is a table demonstrating the symptoms of right-sided and left-sided heart failure [Ref]:
Symptoms | Left-Sided Heart Failure | Right-Sided Heart Failure |
| Trouble breathing | Yes | No |
| Cough | Yes | No |
| Fatigue | Yes | Yes |
| General weakness | Yes | Yes |
| The bluish color of fingers and lips | Yes | No |
| Sleepiness and trouble concentrating | Yes | Yes |
| Inability to sleep lying flat | Yes | No |
| Nausea | No | Yes |
| Loss of appetite | No | Yes |
| Abdominal pain | No | Yes |
| Swelling in ankles, feet, legs, abdomen, and neck veins | No | Yes |
| Frequent urination | No | Yes |
| Weight gain | No | Yes |
Many diabetic patients with heart failure do not have any symptoms at all, especially during the early stages.
They may report vertigo, dizziness, sweating, and symptoms of an upset stomach. The astute physician does not miss these symptoms, however, if missed, the patient might die.
| Read: |
How to Diagnose a Patient with Diabetic Heart Failure?
Heart failure is a clinical diagnosis. Any patient with diabetes who presents with shortness of breath, especially on lying down should be investigated for heart failure regardless of age, gender, or other risk factors.
Patients with Diabetic Heart Failure may be investigated as follows:
Risk factors:
Investigate risk factors such as hyperlipidemia, hypertension, IHD, smoking, obesity, and family history of heart disease.
Medical History:
Medical history includes the symptoms of heart failure, previous diagnosis of heart failure, and aggravating factors such as medications that may cause heart failure.
Family History of diabetes and heart diseases:
Inquire about the family history of diabetes and heart failure. Importantly, ask about any family history of heart failure in relatives younger than 30 years of age.
Symptoms of heart failure including atypical symptoms:
The classical symptoms of heart failure include shortness of breath on lying down or at night, exertional shortness of breath, palpitations, chest pain, and leg swelling.
Atypical symptoms may include fatigue, frequent urination at night, dry cough, heartburn, and weight loss.
Cardiovascular and Respiratory Examination:
Chest examination may show bibasal crepitations and wheezing. heart examination may show an S3 gallop rhythm.
Electrocardiogram:
ECG may show findings suggestive of old ischemic heart disease such as Q waves, abnormal rhythms, ST-segment and T wave changes, and small QRS complexes.
Echocardiogram:
An echocardiogram is essential to find the degree of cardiac anatomical defects such as valvular incompetence and wall motion abnormalities.
It is also important to calculate the ejection fraction so as to label the patient as having either a reduced ejection fraction when the EF falls to less than 40 % or a preserved EF when the EF is above 40%
Blood Test N-terminal pro-B type Natriuretic Peptide (NT-proBNP):
Elevated BNP levels exceeding 400 pg/ml is highly suggestive of heart failure in the presence of typical clinical findings.
BNP levels are also done at follow-up to see if the heart failure medications are working perfectly or if their doses need any adjustment.
Chest X-ray:
A chest x-ray may show cardiomegaly, upper lobe diversion, Kerley B lines, and Kerley A lines. In severe cases, patients may have bilateral pleural effusions as well.
Stress Test:
A stress test is rarely done in symptomatic patients. It may be advised on a follow-up visit to look for inducible ischemia.
Cardiac computerized tomography (CT) scan and Magnetic resonance imaging (MRI):
These tests are performed in rare situations when evaluation for detailed cardiac anatomy is required.
Coronary angiogram:
A coronary angiogram is performed to see if the cardiac vessels are patent and have adequate blood flow or not.
Myocardial biopsy:
This is rarely performed to rule out alternative causes. It is not indicated in patients with diabetic heart failure.
| Read: |
The “New York Heart Association classification” of Heart Failure:
This classifies heart failure symptoms into 4 categories
Class I: No Symptoms with normal physical activity. Normal functional Status
Class II: Mild Symptoms with normal physical activity. Comfortable at rest. Slight limitation of functional status
Class III: Moderate Symptoms with less than normal physical activity. Comfortable only at rest. Marked Limitations of Functional Status
Class IV: Severe symptoms with features of heart failure with minimal physical activity and even at rest. Severe limitation of physical activity.
The American College of Cardiology and Americal Heart Association Guidelines:
This stage-based classification system uses letters A to D. The system includes a category for people who are at risk of developing heart failure.
Stage A: Patients at high risk for developing heart failure in the future but with no functional or structural heart disorder
Stage B: A structural heart disorder but no symptoms at this stage.
Stage C: Previous or current symptoms of heart failure in the context of an underlying structural heart problem, but managed with medical treatment
Stage D: Advanced disease requiring hospital-based support, a heart transplant, or palliative care.
| Read: |
Management of Diabetic Heart Failure:
The mainstay of treatment is diabetes control. Below are the effects of diabetes treatments on the risk of diabetic heart failure:
Biguanide (Metformin):
- Associated with better short-term and long-term prognosis in patients with Heart failure
- Associated with reduced mortality in Heart Failure patients
- Reduces cardiac hypertrophy by AMPK-mediated repression of mTOR and as a consequence protein synthesis
- AMPK activation by metformin can stimulate cardiac glucose uptake.
- Metformin is considered the first-line oral antidiabetic drug even in patients with heart failure. However, in diabetic patients with advanced and symptomatic heart failure, it is not indicated.
Sulfonylureas (SU):
- Originally thought to increase mortality in patients with diabetic heart failure.
- No definitive Cardiovascular outcome trial to evaluate the cardiovascular safety of Sulfonylureas vs placebo or other diabetic agents has been conducted.
- Meta-analysis reports no increased Cardiovascular risk with Sulfonylurea’s treatment vs metformin
- A retrospective cohort study reported an increased Cardiovascular risk in patients on Sulfonylureas vs. metformin or DPP4 inhibitor
- No definitive Cardiovascular outcome trials examining Sulfonylureas in Heart failure have been conducted
- However, Glyburide, a longer-acting sulfonylurea, and first-generation SU have been found to increase the risk of sudden cardiac deaths in elderly diabetic patients.
Thiazolidinediones (TZDs):
- Reports on the effects of TZDs on Cardiovascular safety are conflicting.
- Beneficial effects were anticipated given improvements in glycemic control, inflammatory biomarkers, Blood pressure, triglyceride levels, and HDL
- The proactive trial showed no reduction in the cardiovascular outcomes in patients on pioglitazone
- A meta-analysis reported an increased risk of Myocardial infarction with rosiglitazone
- IRIS trial reported a lower risk of stroke and Myocardial infarction in patients on pioglitazone vs placebo
- The occurrence of fluid retention and weight gain is a reproducible side-effect of TZD therapy, which precludes its use in NYHA III and IV heart failure.
Glucagon-like peptide-I (GLP-I) receptor agonist:
- Meta-analysis reports no increased risk of heart failure or hospitalization for HF among type 2 diabetics
- A meta-analysis revealed a modest improvement in ejection fraction in heart failure patients
- A trial of GLP-1 agonist in advanced HF revealed a trend toward increased hospitalization in the diabetes mellitus subgroup.
- GLP-1 analogs with proven cardiovascular benefits like Semaglutide, Liraglutide, and Dulaglutide are considered first-line medicines in diabetic patients with CAD.
- Read: Semaglutide Heart Failure Trial: Wegovy STEP-HFpEF Trial
Dipeptidyl peptidase 4 (DPP4) Inhibitors:
- The SAVOR-TIMI-53 Trial reported a significant increase in hospitalization for heart failure in patients on saxagliptin vs. placebo
- EXAMINE and TECOS trials do not reveal increased HF risk
- Experimental studies in humans and animals show improvements in cardiac function when GLP-1 was activated by the DPP4 inhibitor
- DPP-4 knock-out mice showed induction of cardioprotective gene signature post-MI
Sodium-glucose co-transporter 1 and 2 (SGLT1 and 2) Inhibitors:
- SGLT2 improves cardiovascular risk factors (diabetes control, weight reduction, reduction in SBP, and it causes osmotic diuresis resulting in symptomatic improvement)
- EMPA-REG OUTCOME trial reported a reduction in cardiovascular mortality and hospitalization from HF using empagliflozin.
- Empagliflozin and Dapagliflozin have been approved in the treatment of patients with heart failure and preserved ejection fraction or diastolic heart failure.
- CANVAS trial reported similar results for canagliflozin.
- Meta-analysis of cardiovascular events in type 2 diabetics on dapagliflozin reported no increased risk for cardiovascular events.
- SGLT-2 inhibitors are even used to treat patients with heart failure without diabetes.
Insulin:
- Some observational trials have suggested a relationship between insulin use and HF risk.
- This could be the result of increased events of hypoglycemia resulting in adrenaline release or direct water-retaining properties of insulin.
- Cardiovascular outcome trials with long-acting insulin analogs do not demonstrate increased cardiovascular event rate or HF
| Read: |
Management of Diabetic Heart Failure:
The management of stable heart failure is different compared to patients who are acutely sick.
Acutely sick diabetes patients with heart failure require oxygen, diuretics, nitrates, and possibly morphine (to alleviate the dyspnea).
Stable patients with heart failure need medicines that have long-term cardiac beneficial effects and drugs that lower the death rates.
The important drugs that prevent cardiac re-modeling and are effective in the treatment of heart failure in diabetes include:
ACE inhibitors:
- These drugs are considered first-line in the treatment of patients with diabetes and hypertension, heart failure, or nephropathy.
- Enalapril, Captopril, lisinopril etc
- No interaction by Diabetes status
- The benefit of captopril was similar among non-diabetes Mellitus and diabetes mellitus.
Angiotensin receptor blockers:
- Like ACE-I, Angiotensin receptor blockers are also considered first-line in the treatment of patients with diabetes and hypertension, heart failure, and nephropathy.
- They are especially recommended for patients who are allergic to ACE-I.
- Valsartan, Losartan, Irbesartan, Olmesartan, Telmisartan, etc
- Valsartan improved the composite outcome in those with and without diabetes.
RAAS and Angiotensin Receptor Neprilysin Inhibitors:
- Neprilysin inhibitors are a novel class of medicines.
- These drugs are usually given in combination with valsartan (Sacubitril/ Valsartan) because of their association with angioedema.
- Neprilysin is an enzyme that degrades the atrial and brain natriuretic peptides.
- When Neprilysin is inhibited, the levels of ANP and BNP in the blood are elevated and the duration of their action is prolonged.
- These drugs cause diuresis in response to cardiac stretch and improve the ejection fraction and the rates of sudden cardiac deaths in patients with markedly reduced ejection fraction.
- Sacubitril (Usually co-administered with Valsartan as Uperio and Entresto)
β-Blockers:
- These drugs reduce the cardiac workload.
- Bisoprolol, Carvedilol, and Metoprolol ER
- Similar reductions in mortality and hospitalization in DM and non-DM
Mineralocorticoid receptor antagonist:
- These drugs inhibit the cascade of RAAS activation in patients with heart failure.
Ivabradine:
- Ivabradine acts on the SA node and reduces the heart rate without affecting cardiac contractility.
- Ivabradine significantly reduced cardiovascular death or HF hospitalization in patients with and without DM
Implantable Cardioverter-Defibrillator/Cardiac Resynchronization Therapy
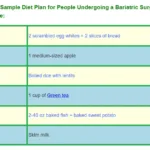
Lifestyle Management
- Lifestyle management should be integral to the care of patients with DM and HF.
- Diabetes Mellitus is linked to obesity, inactivity, and poor dietary choices, which in turn are linked to cardiovascular diseases, including HF.
- Exercise can improve functional capacity for patients with DM and HF.
- Exercise is safe and beneficial in patients with HF and DM. Patients referred to cardiac rehabilitation should be counseled on the importance of adherence to training.
- In patients with HFpEF and obesity, many of whom also have DM, a combined diet and exercise program can improve functional capacity.
| Read: |
In Summary:
Diabetic Heart Failure may occur as a result of long-standing diabetes or as an unrelated disease.
It is important that diabetes patients with heart failure may have subtle symptoms like fatigue and lethargy, dizziness, vertigo, and heartburn.
Early diagnosis and treatment may save the person from long-standing complications and even death.