Here we discuss the complications of the 5 common bariatric surgery complications. The immediate and long-term complications of gastric sleeve and gastric bypass complications years later and during the immediate postoperative period are discussed in detail.
Patients undergoing bariatric surgery can have complications during the surgical procedure, immediately after the surgery, and later even up to 15 years.
The early bariatric surgery complications are mostly because of the change in the anatomy of the gut, wound infection, or bleeding.
Late complications of bariatric surgery that may develop after months to years of the surgery include:
- malabsorption
- adhesions,
- strictures,
- peptic ulcers,
- cholecystitis,
- bacterial overgrowth, and
- vitamins deficiency.
However, the complication rates with the different bariatric surgical procedures vary. Intragastric balloon placement, Adjustable gastric banding, and laparoscopic sleeve gastrectomy are associated with the least number of complications.
On the other hand, gastric bypass surgeries and “duodenal switch” are associated with many complications.
Common Complications of Bariatric Surgery:
Gastrointestinal side effects are the most common. Invasive procedures are associated with complications of surgery such as anastomosis leakage and adhesions resulting in intestinal obstruction later in life.
Lastly, pancreatic exocrine insufficiency and malabsorption are common with some of the procedures.
Here is a list of the complications of weight loss surgery:
- Nausea and vomiting
- GERD
- Oesophageal achalasia
- Band slippage and strangulation of the stomach wall
- Bleeding
- Anastomotic leaks
- Marginal ulcer formation
- Dumping syndrome
- Nutritional deficiency
- Pancreatic exocrine insufficiency
- Nutritional deficiency
- Protein mal nutritional
- Adhesive obstruction
5 Common Weight Loss Surgeries
There are five different weight loss procedures that are commonly practiced. These include:
- Intragastric balloon placement
- Laparoscopic Adjustable gastric banding
- Laparoscopic Sleeve Gastrectomy or Gastric Sleeve Surgery
- Roux-en-Y Gastric Bypass surgery
- Duodenal switch with biliopancreatic diversion
Each of the above weight loss procedures is associated with different complications.
Complications of Gastric Balloon:
The placement of the intragastric balloon is done through an endoscope. The latest technique allows the patients to swallow the balloon and is the least technical of all the procedures.
Common complications of intragastric balloon placement are nausea, vomiting, GERD, gastric ulcer, and balloon migration.
Gastric ulcer and balloon migration can be serious and may require surgical correction.
The frequency of each of the complications associated with intragastric balloon placement is tabulated here:
Complications of Gastric Balloon | |
| Complications | Percentage |
| Nausea and vomiting | 29% |
| GERD | 18.3% |
| Early removal of the intragastric balloon | 9.1% |
| Gastric ulcer | 2% |
| Balloon migration | 1.4% |
Nausea and vomiting (29%)
Nausea and vomiting are common in patients who undergo an intragastric balloon placement. It has been reported in up to one-third (29%) of the patients undergo a gastric balloon placement.
This is because of the presence of an already inflated balloon that occupies some volume of the stomach.
Some patients may not tolerate it and may request early removal of the device.
How to treat nausea and vomiting caused by an intragastric balloon?
This is intolerable for some patients. It may require early removal of the device if the symptoms are severe and totally intolerable.
Those patients with mild symptoms of nausea and vomiting may be treated with short-term antiemetics, antacids, and proton pump inhibitors like omeprazole, pantoprazole, and lansoprazole.
GERD (Gastroesophageal Reflux Disease) (18.3%):
This is another non-life-threatening complication of intragastric balloon placement. Patients report symptoms of retrosternal burning or heartburn and may have altered taste and sour brash.
GERD is reported in about 18% of the patients who undergo intragastric balloon placement.
How to Treat GERD?
GERD can be treated with motility drugs such as metoclopramide, domperidone, and itopride along with an antacid.
Most patients respond to OTC prokinetics and antacids.
Early removal of the intragastric balloon (9.1%)
Sometimes, the device is intolerable for the patient and may require early removal of the device. This is usually because of persistent non-tolerable nausea and vomiting.
How to treat:
If symptoms do not respond to medical treatment, then removal of the device is the only remedy.
Gastric ulcer (2%):
Gastric ulcers can develop due to the direct contact of the foreign object (in this case, the intragastric balloon) with the stomach wall.
The gastric balloon also exerts continuous pressure on the stomach mucosa and may not allow it to heal itself.
A gastric ulcer may bleed to death if it erodes a major vessel. In rare cases, the patient can develop gastric perforation for which he may require surgery.
How to treat gastric ulcers?
Initial assessment with upper GI endoscopy is important t assess the depth and degree of ulceration.
In the initial stages, simple treatment with antacids and PPIs like omeprazole is the treatment of choice. If an ulcer has eroded the vessel it will require endoscopic ablation.
Ballon migration (1.4%):
Balloon migration affects about 1.4% of the people who undergo this procedure. Although it is relatively uncommon it can be life-threatening.
Because balloon migration can lead to gut obstruction, perforation, and peritonitis, it is one of the serious complications of intragastric balloon placement.
Balloon migration usually occurs if the balloon is not sufficiently inflated or has deflated because of some reasons.
Treatment of balloon migration is usually surgical removal of the balloon.
How to treat balloon migration?
If the balloon has not migrated beyond the duodenal segment it can be treated with upper GI endoscopy.
If it has traveled beyond the reach of an endoscope, it will usually require surgical removal.
Initial assessment will require X-rays, Ultrasound, and CT scan of the abdomen to assess elements of obstruction and peritonitis.
Surgery is the last resort in case of non-relieving obstruction and peritonitis. Enterotomy will be required in case of removal if it is stuck at any point.
Lap Band Complications (Adjustable Gastric Banding):
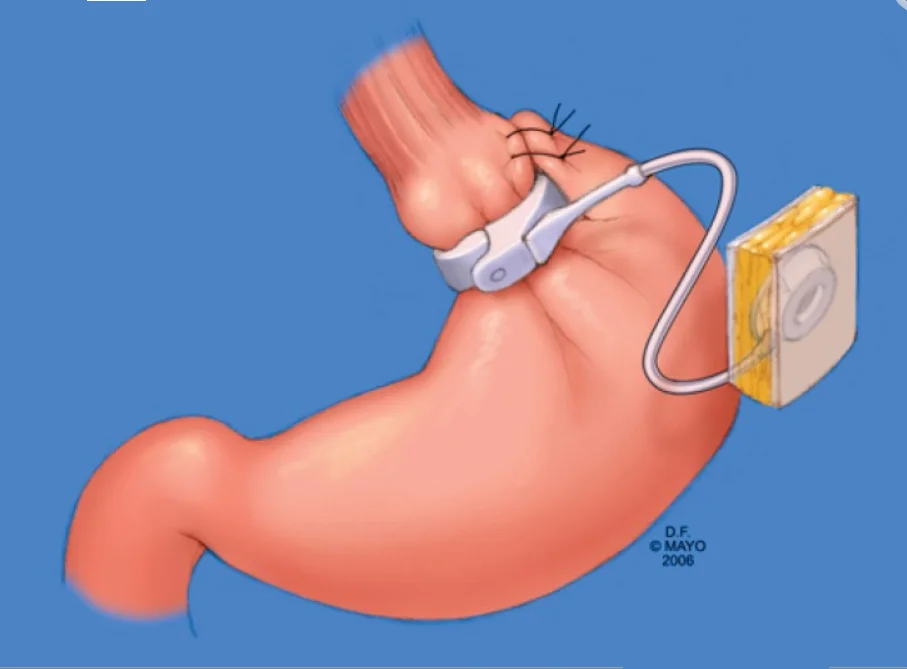
The adjustable gastric band or gastric banding is a minimally invasive bariatric surgical procedure. It does not require the resection of the stomach.
An inflatable band is placed around the upper part of the stomach that can be easily adjusted according to the patient,t’s tolerabi,lity and required weight loss [Ref]
Adjustable gastric banding or Lap band or gastric band has some minor and major complications.
Minor complications (22%)
Minor complications of Lathe p band or adjustable gastric banding include port disconnection, port-site hernia, and port-site infection.
The relative frequency of each of these procedures is tabulated here:
Minor Complications of Adjustable Gastric Banding (22%) | |
| Complications | Percentage |
| Ports disconnection | 19.5% |
| Hernia | 4.9% |
| Port site infection | 2.4% |
Port Disconnection (19.5%)
As this band is adjustable which weight loss can be controlled somewhat. The port may get disconnected so inflation and deflation of the band will not be feasible.
How to manage port disconnection:
Surgical correction is the only option for a malfunctioning device.
Port site hernia or Incisional hernia (4.9%)
This is the formation of a hernia in the post-op period in the laparoscopic port area. This commonly forms in umbilical port insertion sites, but can happen at any site.
How to manage port-site hernia?
This complication can be avoided if proper closure of the port site is done during surgery. Once a hernia develops t,hen the only option is surgical correction. It may or may not need a prosthetic mesh.
Port site infection (2.4%)
The Port for saline infusion lies in the subcutaneous plane in the epigastric area. As this is a foreign body, the risk of infection is always there.
How to manage port-site infection?
In the case of simple mild to moderate infections, oral antibiotics and good hygiene are sufficient. If an abscess develops then it will require surgical drainage and intravenous antibiotics.
Major complications (39%) of Adjustable Gastric banding (Lap Band):
Major complications may endanger the patient’s life and nerequireimely diagnosis and treatment. The five common major complications of LAGB or laparoscopic adjustable gastric banding are tabulated here:
Major Complications of Adjustable Gastric Banding (39%) | |
| Complications | Percentage |
| Reoperation | 59.8% |
| Band erosion | 28% |
| Pouch dilation | 11% |
| Band infection | 1.2% |
| Perforated bulbar ulcer | 1.2% |
Reoperation (59.8%)
Because of numerous reasons, most patients who undergo LAGB require at least one surgery. This may be because of sub-optimal results or insufficient weight loss o,r major complications like band slippage and erosion.
How to manage?
In this case, management depends upon the reason for re-operation.
Band erosion (28%)
In the long term continued inflation of gastric ballon will lead to ischemia of the stomach wall and erosion of the stomach wall.
How to manage.
This complication is usually not recognized until it’s too late. Hence, proper attention is required to avoid overinflation as it can be avoided.
If band erosion occurs, the patient will develop pain and hemoptysis. Immediate deflation of the band and early endoscopy to establish the diagnosis are required.
Pouch dilatation (11.0%)
When the band is applied and inflated, it creates a small primary pouch for food to be stored in the upper part of the stomach.
Sometimes, if patients do not follow the nutritional guidelines and ingest large quantities of food or the band is inflated too much and the passage for food is narrowed, this will lead to dilation of the stomach pouch along with dilatation of the lower esophagus.
Pouch dilation can be prevented by properly following the nutritional guidelines and limiting food intake.
Band infection (1.2%)
Sometimes the band can get infected as it acts as a nidus for infection.
How to manage?
The management option is the same as any other intraabdominal infection. But it may require the removal of the band through surgery.
Perforated bulbar ulcer (1.2%)
This happens on the inside of the stomach wall where the band is inflated. This is also because of continued partial ischemia.
How to manage a perforated bulbar ulcer?
In this case, the patient will present with severe abdominal pain with board-like abdominal rigidity because the stomach contents are highly irritative and cause severe peritonitis.
This will require surgery with the removal of the band and closure of the perforation with omentopexy to strengthen the perforation site.
Early and Late Complications of Gastric Sleeve (Laparoscopic Sleeve Gastrectomy)
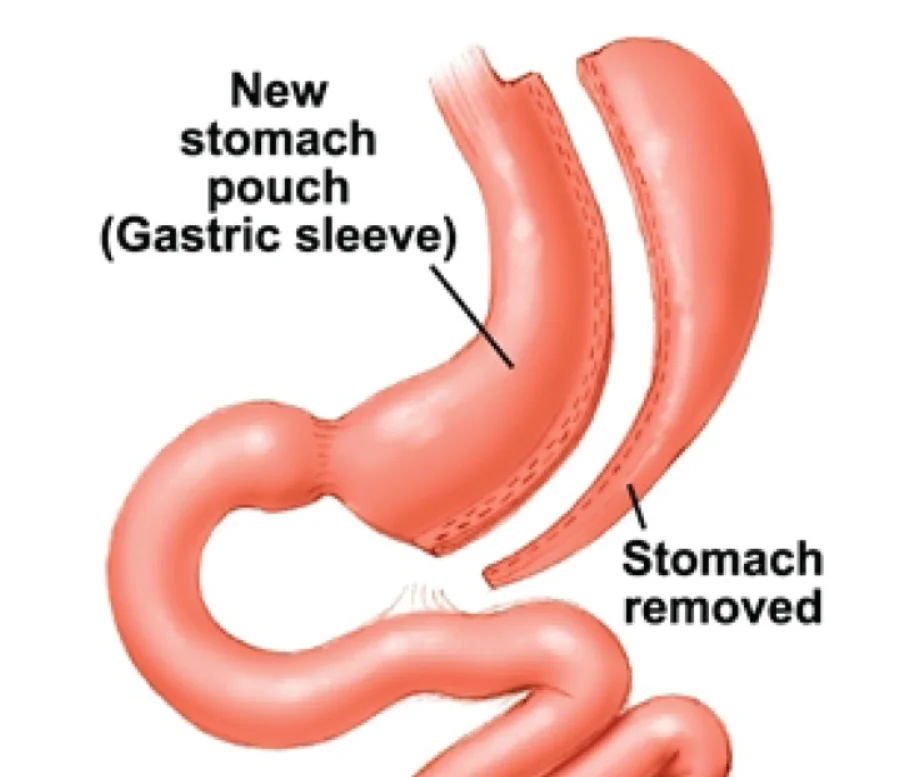
Early complications of Gastric Sleeve:
Early complications of laparoscopic sleeve gastrectomy usually refer to any complication that occurs within the first two to four weeks of the procedure.
Most of these complications are surgery-related rather than the effects of the procedure.
Common early complications of Gastric Sleeve include:
- Bleeding
- Staple line leakage
Bleeding (1 – 6%)
Bleeding is usually seen from the staple line. Bleeding can occur in the intestinal lumen or outside the intestinal lumen.
How to manage bleeding after gastric sleeve?
Intra luminal bleeding can be controlled via an endoscope whereas, extra luminal bleeding or bleeding that occurs in the abdominal cavity requires surgical intervention.
- Staple line leakage:
Leakage of gastric contents through staple lines is a drastic complication. It can be seen as early as the third post-op day or as late as the 8th post-op day. This will lead to an intraabdominal collection and peritonitis.
How to manage staple line leakage?
The treatment option depends on the size of the leakage. Small leaks can be treated with an endoscope, where they can be closed easily.
Whereas large leakage will require surgical closure with a buttressing suture line. The intra-abdominal collection will require drainage either through an image-guided approach or through a surgical approach.
If surgery is undertaken, then the collection is drained and the cavity is washed. Postoperatively, a drain is placed to drain any collection that is left and to wash the wound.
Late complications of Gastric Sleeve Surgery (laparoscopic sleeve gastrectomy):
Late complications of LSG are defined as those complications that occur after 30 days of the surgical procedure.
Late complications can arise as a result of the surgical procedure or because of the effects of LSG on the body.
Common late complications of LSG (laparoscopic sleeve gastrectomy) include:
Late complications of LSG | ||
| Complications | Percentage | |
| GERD | 47% | |
| Stricture formation | 3.5% | |
| Nutritional deficiency | Nutrient | |
| Vitamin D deficiency | 23% | |
| Zinc | 14% | |
| Iron | 3% | |
| Folic Acid | 3% | |
| Vitamin B 12 | 3% | |
GERD (47%)
GERD (gastroesophageal reflux disease) is a common complication of patients who have had LSG. About half of the patients who have had LSG report the symptoms of GERD.
Patients may develop heartburn, retrosternal chest pain, burping, and sour brash.
How to manage GERD?
GERD can be managed by modifying diet, avoiding meals immediately before going to bed, and walking for a while after taking a meal.
Treatment with an antacid or a PPI (omeprazole, pantoprazole, etc) is usually indicated to relieve the symptoms.
Stricture formation (3.5%)
This is another serious complication that may develop in patients undergoing laparoscopic sleeve gastrectomy. This is usually because of swelling or edema in the stomach wall, but this can also occur as a result of kinking of the stomach.
How to manage stricture formation?
The treatment option is correcting the problem through an endoscopic approach.
Nutritional deficiency:
Deficiency of nutrients can occur because of several reasons, including inadequate diet and inadequate absorption. Nutritional deficiency is more common with other advanced procedures like gastric bypass and duodenal switch.
Common nutrient deficiencies that may occur in patients undergoing LSG include:
Nutrient deficiency | Percentage |
| Vitamin D deficiency | 23% |
| Zinc | 14% |
| Iron | 3% |
| Folic Acid | 3% |
| Vitamin B 12 | 3% |
How to manage nutrient deficiency?
Nutritional assessment before surgery is essential. Patients are usually advised adequate, balanced, vitamins and minerals-rich diet before and after the procedure.
Supplementation of vitamins and minerals is usually necessary for all patients who undergo a bariatric surgical procedure.
Gastric Bypass Complications:
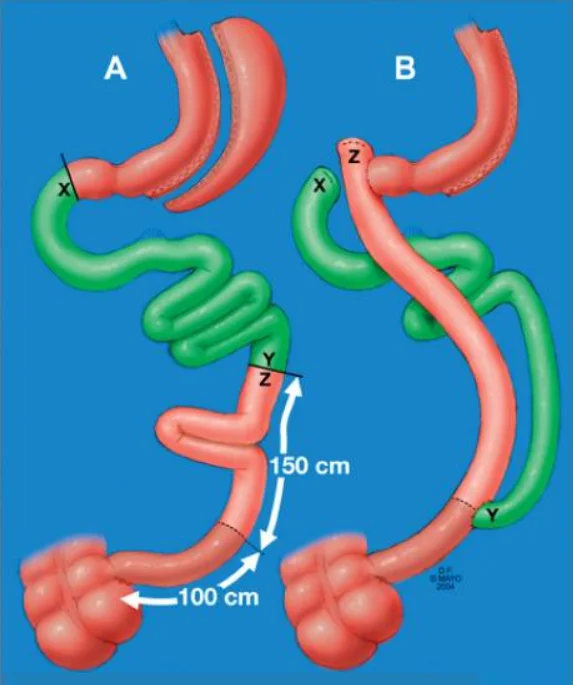
Compared to LSG (Laparoscopic sleeve gastrectomy), this is a more invasive procedure and is associated with more complications.
Common complications of the Gastric Bypass procedure include:
Complications of Gastric Bypass Surgery | ||
| Wound infection | 4.7% | |
| Ileus | 1.4% | |
| Bleeding | Intra-abdominal | 2.2% |
| Gastrointestinal | 1.1% | |
| Leaks | 2.5% | |
| Stricture formation | 4.7% | |
| Marginal ulcer | 0.7% | |
| Pancreatic exocrine insufficiency at 1 year | 9.1% | |
| Nutritional deficiency | Variable | |
| Second surgery | Cholecystectomy | 17% |
| Laparoscopic adhesiolysis | 15% | |
| Umbilical hernia repair | 10% | |
Wound infection (4.7%):
As this is a more invasive and contaminated surgery, the risk of infection is always higher than in other surgeries.
Infections can occur as a result of minor leakage during anastomosis can lead to infections.
How to manage?
Wound infection is treated with antibiotics and or surgical drainage of any collections as mentioned for other procedures.
Ileus (1.4%):
In the post-op period, some patients may experience ileus more than usual. This is because of gut handling, the gut goes into a state of paralysis.
Ileus can get worse with prolonged gut handling, infection, ischemia, and hypokalemia.
How to manage Ileus?
Early mobilization and treatment with pro-kinetics are important. Serum electrolytes especially potassium correction is of utmost importance.
Bleeding intra-abdominal (2.2%) and gastrointestinal (1.1%)
This is usually seen from the staple line. Sometimes the staples injure the blood vessels without properly occluding them. This leads to bleeding. Bleeding can occur in the lumen or outside the lumen into the peritoneal cavity.
How to manage bleeding after Gastric bypass surgery?
Mild bleeding is usually managed conservatively with adequate hydration, PPIs, and antifibrinolytic drugs like tranexamic acid.
Severe bleeding may require surgical correction and re-operation.
Leaks (2.5%):
Anastomotic leaks are a dangerous complication associated with this procedure. It can be contained or may present with generalized peritonitis and sepsis.
How to manage anastomotic leaks?
Leaks are usually managed conservatively with antibiotics. However, surgical exploration may be necessary.
Stricture formation (4.7%)
Stricture formation is usually seen in patients who undergo gastro-jejunostomy anastomosis. This can be a serious complication and patients may develop intestinal obstruction manifesting as persistent vomiting and abdominal pain.
How to manage stricture formation?
In this case, management varies according to the cause. If it is because of edema of the surrounding tissues, then the restriction of fluids in the post-operative period and the use of diuretics will correct the problem.
But if the anastomosis lumen is narrow, it will require endoscopic dilation. In some cases, if the endoscopic approach fails then surgery is done and reconstruction of the anastomosis is performed.
Marginal ulcer (0.7%)
This is seen at the anastomosis site of gastro-jejunostomy. It is not a serious complication, but it can result in stenosis of the anastomotic lumen if left untreated.
How to manage marginal ulcers?
Treatment of marginal ulcers is the same as other ulcers. High-dose PPIs and antacids may heal marginal ulcers rapidly.
Pancreatic exocrine insufficiency (9.1%):
The development of pancreatic exocrine insufficiency after a bariatric procedure especially gastric bypass is a common complication.
It is more common in all types of bariatric surgical procedures that bypass the stomach or reduces its volume. This is a long-term complication that will manifest as malnutrition.
How to manage pancreatic exocrine insufficiency?
This is an irreversible change in the pancreas. However, it can be avoided to some degree with the use of pancreatic-stimulating foods and supplements that may act as pancreatic digestive enzymes.
Nutritional deficiency after gastric bypass surgery:
As this is a malabsorptive surgery, most patients usually develop a deficiency of micro- and macronutrients in the long run.
Continuous replacement of nutrients and a healthy nutrient-rich diet are usually advised to avoid the deficiency of nutrients.
In one study, 14% of the patients who underwent gastric bypass surgery developed iron deficiency at 2 years, and 27% of the patients developed iron deficiency at 3 years after the gastric bypass procedure.
How to manage nutritional deficiency after gastric bypass surgery?
Pre-operative assessment of nutrient deficiency is important. Correction of the deficient nutrients before and after surgery is done.
The replacement of macronutrients and micronutrients usually continues for life.
Second surgeries:
Patients who undergo gastric bypass surgery usually undergo a second surgery at some point in their lives. The second surgery that the patients may require after gastric bypass surgery includes:
Cholecystectomy (17%):
Because of the rapid weight loss and stagnant bile, which can crystallize, gallstones can form, which may require cholecystectomy.
How to manage gallstones:
Development of gallstones post-malabsorptive surgeries is common, which is why prophylactic cholecystectomy or sometimes chemoprophylaxis for gallstones is recommended.
Patients may be advised to take ursodeoxycholic acid to prevent the formation of gallstones.
Laparoscopic adhesiolysis (15%)
Adhesion formation post-bariatric surgery is common in surgeries requiring extensive dissections and multiple resections, and anastomosis.
Umbilical hernia repair (10%)
Port site herniation is a common side effect in laparoscopic surgeries. As the umbilicus is a congenitally weaker point, herniation is common, resulting in an umbilical hernia.
Complications of Duodenal Switch and Biliopancreatic Diversion:
This is the most invasive bariatric surgical procedure and is associated with significant mortality compared to other bariatric surgical procedures.
Early complications of Duodenal switch with a biliopancreatic diversion:
Early complications of the Duodenal switch with biliopancreatic diversion are those that occur within the first month of the surgery or during the surgery.
Most of these complications are a result of faulty procedure techniques, inadequate sterilization, and an inexperienced surgeon.
Wound infections (15%)
Infection of the port site and infection from leaks are major complications in this procedure.
Infections are managed with intravenous antibiotics and wound lavage.
Dumping syndrome (6%).
This complication is because of the resection of the pylorus. Pylorus acts as a valve that controls the food outlet into the small intestine. Removal of the pylorus leads to dumping of food, leading to dumping syndrome.
Patients can develop diarrhea, dizziness, and hypotension immediately after eating a meal, especially meals that are rich in osmotically active food particles such as simple carbohydrates and heavy meals.
How to manage dumping syndrome?
Dumping syndrome can be managed with small meals. Meals containing free sugars will worsen the condition and should be avoided.
Late complications of Duodenal switch with a biliopancreatic diversion:
Late complications can occur either as a result of the procedure itself or as a result of the effects of the procedure.
Common late complications of Duodenal switch with biliopancreatic diversion include:
Complication | Percentage |
| Bacterial overgrowth | 27% |
| Incisional hernia | 15% |
| Peptic ulcer | 15% |
| Acute cholecystitis | 6% |
| Afferent loop obstruction | 3% |
| Protein malnutrition | variable |
Bacterial overgrowth (27%)
This occurs as an afferent limb is bypassed for food digestion. This limb acts as a blind loop, which will lead to stagnation of contents that leads to bacterial overgrowth.
How to manage bacterial overgrowth?
Bacterial overgrowth is treated with gut antiseptics such as Rifaximin (Xifaxin) or with oral or intravenous antibiotics.
Incisional hernias (15%):
This complication is multifactorial and ranges from patient factors to the surgical techniques used.
How to manage?
Management depends on the size of the hernial defect. Surgery is the only option, but the decision of placing mesh depends on the size of the defect.
Peptic ulcer (15%):
This is another complication that can be serious if not dealt with on time. As it may lead to complications.
How to manage
Management of peptic ulcers depends on the ulcer size and depth. Initial treatment is with PPIs. If required, endoscopic treatment may be needed.
Acute cholecystitis (6%)
The formation of gallstones in malabsorptive surgeries is a common complication. That is why prophylactic cholecystectomy is performed at the time of surgery if the patient has gallbladder sludge or gallstones.
How to manage?
Prophylactic cholecystectomy is recommended for patients who have gallstones or sludge. Prophylactic ursodeoxycholic acid 500 mg twice daily is recommended for patients for 6 months.
The prophylactic use of Ursodeoxycholic acid reduces the incidence of gallstones.
Afferent loop obstruction (3%)
This can be a serious complication if not treated on time. If left untreated this blind end may burst open and lead to peritonitis.
Protein Malnutrition.
This is a major complication of both procedures. Pre-operative assessment is required for protein deficiency.
Protein malnutrition may get worse after the surgery. A high protein and nutrient-dense diet is advised, however, in patients who do not recover from protein malnutrition, reversal of the procedure may be indicated.
How to manage?
Initial management requires the patient to have nutritional support through parental and enteral routes. If the patient does not respond to the dietary supplementation, then reversal of surgery is recommended.
- Premium Ingredients: Our tea blend features high-quality Berberine, aromatic Oolong, and refreshing Mint, all organicall…
- Mint Flavored: Enjoy the cool, crisp taste of mint that perfectly complements the robust flavors of Berberine and Oolong…
- Unsweetened with Zero Calories: Crafted for those who appreciate the natural flavors of tea, our blend is completely uns…
- COMPLETE BARIATRIC MULTIVITAMINS. Formulated for post bariatric surgery patients nutritional needs. Gastrectomy, gastric…
- POST BARIATRIC SURGERY MUST HAVES. An effective bariatric multivitamin capsule with iron supplement for women and men. I…
- 21 ACTIVE INGREDIENTS, with 18 at 100% DV including niacin, thiamin & iron. Vitamin A, C, D, E, B6, B12, folate, ribofla…

- Our Complete Chewable Bariatric Multivitamin is an all-inclusive vitamin to support your nutritional needs. Each bottle …
- This supplement is extremely easy to take! The suggested use is to take 4 chewable tablets per day. This formula is chew…
- Great tasting flavor! This Bariatric Multivitamin is packed with nutrients so that no other supplement is needed.